
By Marie Garlock
Stage IV cancers are not a free license to lower healthcare quality, gut drug safety, or bankrupt families made vulnerable by difficult diagnoses. People with stage IV cancers have vital wisdoms to impart about the need for equitable access to quality, affordable healthcare for all, and for thorough, thoughtful reviews by the FDA for drugs and devices they’ll use.
My mom and best friend Barbara Bosma Garlock first got stage I breast cancer at 44, and like many families in our situation, we didn’t really need to know much about cancer advocacy until her diagnosis. As she underwent cancer treatments, our family began to realize that Barbara’s priorities were powerfully reflected in Breast Cancer Action’s pursuit of health justice.
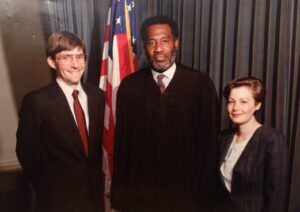
Whether facing daunting personal challenges or opportunities to stand in the gap for others facing injustices, my mama’s refrain was: “May my life be of service.” As a young woman, Barbara worked full time while going to college, and toted me along in an infant seat while she turned in grad school papers. She became a healthcare lawyer to help vulnerable populations who needed patient advocates, and ended up improving hospitals’ ethics guidelines for then-taboo issues like HIV/AIDS, teen pregnancies, and end of life care. In the 1990s, as she became the youngest woman and first working mom to become partner at her southern firm, Barbara brought a unique passion to ensuring patient-centeredness and equitable treatment under the law—but this commitment wasn’t just a personality trait. It arose from her lived experiences growing up in poverty in D.C., in majority-Black neighborhoods that were underserved, polluted, and made dangerous by infrastructure crumbling under policy racism and classism.
 After a cancer diagnosis, my mom went back to work and started a mid-career shift toward fulfilling her dream of a legal aid and patient support clinic model. Yet, like 1/3 of women with early stage breast cancers in the U.S., she experienced cancer’s frustrating return just 2 years later, at 46. When my little brother was just 13, our mom Barbara had stage IV metastatic breast cancer in her spine, femurs, and an ovary. The disease had spread unchecked for months while she was in a healthcare coverage gap, 3 years before the ACA passed. Pre-existing condition discrimination meant prohibitively high costs for the cancer blood assays Barbara needed but skipped, due to unfathomable annual insurance premiums above $40,000 for our family of 4, and a cap at $100k lifetime benefits—a benchmark quickly reached if the bankruptcy-level costs of cancer treatments are in the mix!
After a cancer diagnosis, my mom went back to work and started a mid-career shift toward fulfilling her dream of a legal aid and patient support clinic model. Yet, like 1/3 of women with early stage breast cancers in the U.S., she experienced cancer’s frustrating return just 2 years later, at 46. When my little brother was just 13, our mom Barbara had stage IV metastatic breast cancer in her spine, femurs, and an ovary. The disease had spread unchecked for months while she was in a healthcare coverage gap, 3 years before the ACA passed. Pre-existing condition discrimination meant prohibitively high costs for the cancer blood assays Barbara needed but skipped, due to unfathomable annual insurance premiums above $40,000 for our family of 4, and a cap at $100k lifetime benefits—a benchmark quickly reached if the bankruptcy-level costs of cancer treatments are in the mix!
Later, my mom got healthcare insurance again, but in ways that caused injury and ultimately death, Barbara was left unprotected by the FDA because of its more recent, repeated approvals of drugs and devices that do not meet meaningful research standards for improving breast cancer patients’ health outcomes.
In my family’s case, my mom Barbara had an appendix rupture from the drug Avastin. Its usage for breast cancer was later revoked by the FDA because it was found to cause organ and GI perforations, heart issues, and strokes in patients, and people on the drug had higher death rates over time than if they’d not taken it. Because of Avastin, on Christmas Eve, my mom spent 11 hours in the ER with a painfully ruptured organ before she and my dad were seen. I’ll always remember Barbara’s mission once she was set up in her hospital room post-surgery—she wanted me to deliver presents that were yet to be wrapped. Attached to IV tubes, she scooted around the room with scissors, tape, and her characteristic persistence to make sure “cancer doesn’t keep getting in the way of our joy”! Especially on days she hoped to spend with her kids.

A few years later, our family was in a time of increasing stress when a healthcare insurer refused to cover a well-studied radiation treatment (with 50 years’ worth of solid data). While awaiting approval, the toxicities built up from another more recent cancer treatment called Gemzar (Gemcitabine), used off-label for breast cancer in ways not adequately studied by the FDA. In my mom’s case, Gemzar toxins accumulated and caused a sudden and visceral liver failure, and she was given just 2 weeks to live. I’ll always remember the power and grace she infused us with in that short window. Barbara had a 53rd birthday party with 100-plus guests to whom she gifted her favorite books and sacred poems, scarves and jewelry, art-making supplies, and reasons to laugh (and cry, but in good company). Because of who she was, there was much beauty, but because of Gemzar, there was also real trauma in those dense days in which my mom died from a breast cancer treatment. I want no one else to experience such preventable pain.
Several months later, I worked up the bravery to follow up on what Barbara’s oncologist had hinted at—that she’d never seen anything quite like this, and that Gemzar had likely taken a turn for the worse in my mom’s system as, based on location, the cancer metastases alone could not have produced liver failure. At the time, we’d decided not to bother my mom with yet another test to see what had caused the liver failure, since she only had a few cognizant days left before the liver bile built up in her system and caused death. My skin was hot with nausea, shame, and anger as I read published studies and physicians’ reports of adverse events. In a coffee shop, between completing my grad school assignments, I learned tearfully that more than 6,000 had died among 22,000-plus reported adverse events while on Gemzar/Gemcitabine, including from issues like sudden liver failure. To date, the FDA has not followed up on any of these reports in the form of a post-market study of Gemzar/Gemcitabine.
Like so many others, I got a crash-course in cancer advocacy over the seven years my mom had stage IV breast cancer. I’ve stayed involved with Breast Cancer Action as inspired by Barbara’s experiences as a patient and advocate, and by the patients, caregivers, and clinicians who are part of a remarkable mass movement in my home state of North Carolina, called “Moral Mondays” (now the nationwide Poor People’s Campaign). Six years ago, I was brought on as a “Community Leader for Change” with Breast Cancer Action, and started bringing educational resources, advocacy materials, and outreach opportunities to regional health conferences. In 2015, as a volunteer representative of Breast Cancer Action, I attended a few of the National Center for Health Research’s trainings for patient advocates in Washington, D.C.
 At these PCORI grant-funded trainings, I met a coalition of diverse patients and caregivers with whom I finally learned I was not alone. From their own lived experiences, so many attendees knew the grief and frustration I felt from watching a loved one suffer or die because of an understudied medical device or pharmaceutical drug that poisoned or hurt them.
At these PCORI grant-funded trainings, I met a coalition of diverse patients and caregivers with whom I finally learned I was not alone. From their own lived experiences, so many attendees knew the grief and frustration I felt from watching a loved one suffer or die because of an understudied medical device or pharmaceutical drug that poisoned or hurt them.
In D.C., participants learned about various conflicts of interest that matter to patient safety. One of many things we explored were the FDA’s inner-workings and previously foreign-to-me terms like “surrogate endpoints”, “substantial equivalence for devices”, and “fast tracked” approvals. Afterward, several participant cohorts started the USA Patient Network, a 501c3 non-profit which, today in 2020, consists of patients and families united by advocacy and education to ensure medical treatments that involve drugs or devices are safe, effective, and affordable.
Externally, USAPN works to keep an eye on legislation and Congressional budgets, FDA hearings, and patient advocacy coalition-building opportunities. Refreshingly, USAPN members find connection across diseases and disorders—from users of birth control, anti-depressants, or cancer drugs to patients with implants for breasts, knee or hip replacements, or surgical mesh. We’re motivated by an earnest will to see no more patients and families suffer from regulatory gaps or science designed to tell only half-truths—and to see, in our lifetimes, drug and device approval processes that actually center grassroots patient input.
To be clear: none of us in USAPN seem to arrive or depart with a chip on our shoulder about the FDA, or with “anti-drug” or “anti-device” perspectives. We deeply believed these treatments would make us or our loved ones less sick and less in pain, not more so. In fact, USA Patient Network participants tend to have a stubborn hope that the FDA will be restored as an agency that prioritizes patients’ improved health outcomes by approving medical treatments that work.
“We’re motivated by an earnest will to see no more patients and families suffer from regulatory gaps or science designed to tell only half-truths—and to see, in our lifetimes, drug and device approval processes that actually center grassroots patient input.”
In keeping this hope alive, I’ve found that the distinction between grassroots and astroturf patient advocacy is vital. Right now, the FDA hears from too many patients whose stories are hand-picked by pharmaceutical sponsors for their focus on rushing drugs to market, even before researchers know if these drugs are safe for patients in the long term or if they work as labeled. Biopharma-supported “astroturf” patient stories are wedged into most hearings in which the FDA decides on research design and treatment approvals, because such pre-selected testimonies are glossy and “made to size” for drug companies’ (understandably) self-interested goals.
The FDA must hear far more equitably from distributed, grassroots advocates, voluntarily aligned with people-driven, patient-accountable groups like USAPN, Patient Safety Action Network, Advocating Safety in Healthcare E-Sisters, Medical Device Problems, and from watchdog entities like NCHR: The Voice for Prevention, Treatment, and Policy, Consumer Reports Advocacy, and Breast Cancer Action, among others. Shared of our own accord, our authentic patient testimonies are a compass for needed knowledge that cannot be silenced, even as we face down profitable multinational corporations whose only accountability is to shareholders, or a new breed of regulators who, alongside a broader public influenced by drug advertisements, tends to automatically equate a drug’s efficacy with how innovative or new the drug is.
To this end, I’ve been shocked to learn about the trojan horse of “surrogate endpoints” in FDA drug reviews. Historically, any randomized controlled trials (RCTs) that fit the gold standard of clinical study held up by the FDA and peer-reviewed journals must take into account at least 1 of 3 ways any new drug improves upon existing drugs: (1) It lengthens overall survival (people who take the drug live longer than those who don’t); (2) It improves quality of life (with less toxic or fewer side effects than similar drugs; or (3) It has a lower cost for consumers (it’s produced more affordably than current drugs). But surrogate endpoints actually “sub in” for clinical drug trials’ gold standard goals by zooming in too far on pre-selected physical effects, such as tracking if a particular tumor in someone’s body expands, slows, or stops growth in a 6- or 12-month period. The problem with surrogate endpoints is that we’ve lost sight of the forest for the trees—a shrunken or stable tumor does no good in the body of someone who dies prematurely from the drug itself. The best example of this is Avastin, which shrunk tumors and provided 3-4 weeks of additional life to breast cancer patients within 1 year of clinical trials. This brought excitement, a “breakthrough therapy” designation for Avastin, fast track approval, and eagerness among cancer researchers to see the drug prescribed in wider markets. But beyond 1 year of use, the drug injured and even killed patients with metastatic breast cancer, and overall survival time (length of life) was reduced for people who took Avastin.
“Right now, the FDA hears from too many patients whose stories are hand-picked by pharmaceutical sponsors for their focus on rushing drugs to market, even before researchers know if these drugs are safe for patients in the long term or if they work as labeled.”
Despite clear patterns like this, cancer treatments approved by the FDA in the last 2 decades are increasingly reliant on surrogate endpoints for one reason: they speed up the timeline of clinical trials. That’s an understandably attractive corner to cut for pharmaceutical companies and biotech researchers, because less time in a clinical trial means less money spent, fewer staff to administer it, and a quicker path to market and thus profit. But FDA cancer drug reviews aren’t just obscure “hoops to jump through”—they matter in life and death ways to everyday cancer patients like my mom, and to oncology physicians who’d rather be confident that the drugs they prescribe have been rigorously studied by the FDA and are more likely than not to improve patients’ lives.
To date, the FDA’s stated commitments to patient centeredness don’t have any real enforceability when it comes to how clinical trials are run, because the FDA is not yet including any patients in working groups and advisory boards at the investigational new drug (IND) stage, when trial design standards are decided. And when it comes to people with advanced cancers, the FDA is missing out on hearing from patients who are genuinely free from conflicts of interest.
 In a decade of research interviews and focus groups I’ve conducted with hundreds of participants, I’ve found that people with advanced cancers want helpful treatments, not just innovative treatments that don’t actually help. Contrary to common assumptions that drug industry players perpetuate in popular media, so many current and former Breast Cancer Action members have shown us that people with metastatic cancer are not machines bent on quantity of survival “or else,” willing to endure excruciating harms just for a pulse. Nor are advanced cancer patients just “pitiable” examples of bad luck, who should feel thankful to get whatever is thrown at them when it comes to cancer treatments.
In a decade of research interviews and focus groups I’ve conducted with hundreds of participants, I’ve found that people with advanced cancers want helpful treatments, not just innovative treatments that don’t actually help. Contrary to common assumptions that drug industry players perpetuate in popular media, so many current and former Breast Cancer Action members have shown us that people with metastatic cancer are not machines bent on quantity of survival “or else,” willing to endure excruciating harms just for a pulse. Nor are advanced cancer patients just “pitiable” examples of bad luck, who should feel thankful to get whatever is thrown at them when it comes to cancer treatments.
Stage IV cancer patients’ hospital gowns don’t come with a target sign to hook to their backs for “anything goes” treatments. Or, as my mom would often quote (hilariously) from Monty Python films: “I’m noooot deeead yet!”
“To date, the FDA’s stated commitments to patient centeredness don’t have any real enforceability when it comes to how clinical trials are run, because the FDA is not yet including any patients in working groups and advisory boards at the investigational new drug (IND) stage, when trial design standards are decided.”
My mom Barbara was hurt by surrogate endpoints that undermined the safety of breast cancer treatments she received, and I’d like to tell that story wherever it can make a difference for other patients. But I don’t get invited to speak on FDA panels. It’s only because of unique opportunities to participate in advocacy trainings, which BCAction primed me for, that I now know to watch out for federal register announcements and to apply to speak in the “public comment” section of relevant FDA hearings on behalf of USA Patient Network. Grassroots patients’ hard-earned insights must be more than an afterthought at best (or nuisance at worst) when it comes to which clinical trials, drugs, and devices get approved by the FDA, under which terms. And really, grassroots patients’ goals are quite earnest: to prevent similar mistakes and losses from repeating themselves, and to promote transparency and health equity at every turn.
 But everyday cancer patients and their families have enough on our plates, and most of us aren’t taking all-expenses-paid trips to D.C. to make FDA testimonies on behalf of drug companies who’ve coached us to speak about why the drug should be sped through for quick approval and sales. It’s just too hard to keep up for most of us, especially when the stress of being sick is matched by the stress of how to afford one’s treatments, and the fear of which toxic side effects of treatments are worth the gamble. Let alone the sense of isolation that arises if you don’t identify with popular notions of cancer “success”that attach narratives of personal effort or toughness with breakthrough drugs, and turn life itself into something to be “won” instead of honored. And that’s why the FDA needs to center grassroots patient perspectives whenever they’re deciding to take next steps in studying new drugs. The FDA needs to hear from grassroots patients like us about why and how to have equitable stock-taking of which science counts as good enough in clinical trials, every time cancer patients’ lives are on the line.
But everyday cancer patients and their families have enough on our plates, and most of us aren’t taking all-expenses-paid trips to D.C. to make FDA testimonies on behalf of drug companies who’ve coached us to speak about why the drug should be sped through for quick approval and sales. It’s just too hard to keep up for most of us, especially when the stress of being sick is matched by the stress of how to afford one’s treatments, and the fear of which toxic side effects of treatments are worth the gamble. Let alone the sense of isolation that arises if you don’t identify with popular notions of cancer “success”that attach narratives of personal effort or toughness with breakthrough drugs, and turn life itself into something to be “won” instead of honored. And that’s why the FDA needs to center grassroots patient perspectives whenever they’re deciding to take next steps in studying new drugs. The FDA needs to hear from grassroots patients like us about why and how to have equitable stock-taking of which science counts as good enough in clinical trials, every time cancer patients’ lives are on the line.
My Mama Barbara taught me to connect the dots of where people’s struggles come from, not just what they are. In the spirit of Breast Cancer Action and so many justice movements she was part of, Barbara taught me to center the stories of the most-affected communities as we listen for pathways toward social change and policy justice. That means acknowledging that, in 2020, we have a Food and Drug Administration strategically underfunded by the U.S. Congress and fundamentally reshaped to be beholden to private pharmaceutical companies and medical device manufacturers. It also means reckoning with the truth that too many agencies like the FDA, charged with holding public health and safety in balance with the economic interests of business stakeholders, are pressured into a corner by some of our country’s most powerful lobbyists. I want an FDA that can act freely on behalf of the people and the public they are tasked to serve.
“But everyday cancer patients and their families have enough on our plates, and most of us aren’t taking all-expenses-paid trips to D.C. to make FDA testimonies on behalf of drug companies who’ve coached us to speak about why the drug should be sped through for quick approval and sales.”
I hope each reader whose life has been touched by someone with stage IV cancer will take a moment to write to the FDA and share some of you and your loved one’s truths. What might you request that we don’t yet have? Patient-centered drug trials. Transparent, open-door communication between the FDA, private industry, and the public. And most of all that new, FDA-approved drugs will actually and meaningfully improve breast cancer patients’ health.
Take action today by contacting the FDA and adding your voice now.