These disparities in breast cancer stem from a complex interplay of economics, power, racism, and discrimination that lead to a variety of social injustices, including major inequities in healthcare.
Breast Cancer Action (BCAction) recognizes that a number of diverse communities including young, old, gay, transgender, disabled, immigrants, and under-educated are disproportionately and uniquely impacted by breast cancer. However, due to available data (and lack thereof) on inequities in breast cancer, much of the work in this area is focused primarily on race and class.
Over the last 30 years, the gap in mortality from breast cancer between racial groups has widened. Black women are 42 percent more likely to die from breast cancer than white women. Latina and Samoan women are also more likely to die from breast cancer despite the fact that women in these ethnic communities have a lower incidence of the disease compared to white women.
Disparities in breast cancer outcomes among different racial and ethnic communities are based on the inequities of a complex interplay of social and economic factors such as where we live, work, learn, and play, as well as dynamics of power and influence. The important role of social and economic disadvantage, which include injustices in opportunity and access to resources, as well as structural barriers to receiving high quality healthcare, can no longer be ignored.
Conventional solutions to reducing disparities in breast cancer focus heavily on promoting mammography and access to care, and fail to address underlying, persistent social injustices that lead to the differences in outcomes. Institutionalized hurdles; intergenerational trauma that inequitably impacts different communities (also known as weathering); language and cultural differences; discrimination related to class, race, and citizenship; a history of exploitation and medical mistreatment creating a legacy of mistrust of the medical community; lack of available and appropriate services; and transportation to services, all contribute to the growing disparities in outcomes throughout the breast cancer care continuum.
While creating healthcare access for all increases who gets care, the simple expansion of services without a focus on the quality, delivery, and differential care of these services does not eliminate health inequities. Also, moving focus away from an individual’s behavior and lifestyle choices, to issues outside an individual’s control, such as institutional power and discrimination, is vital.
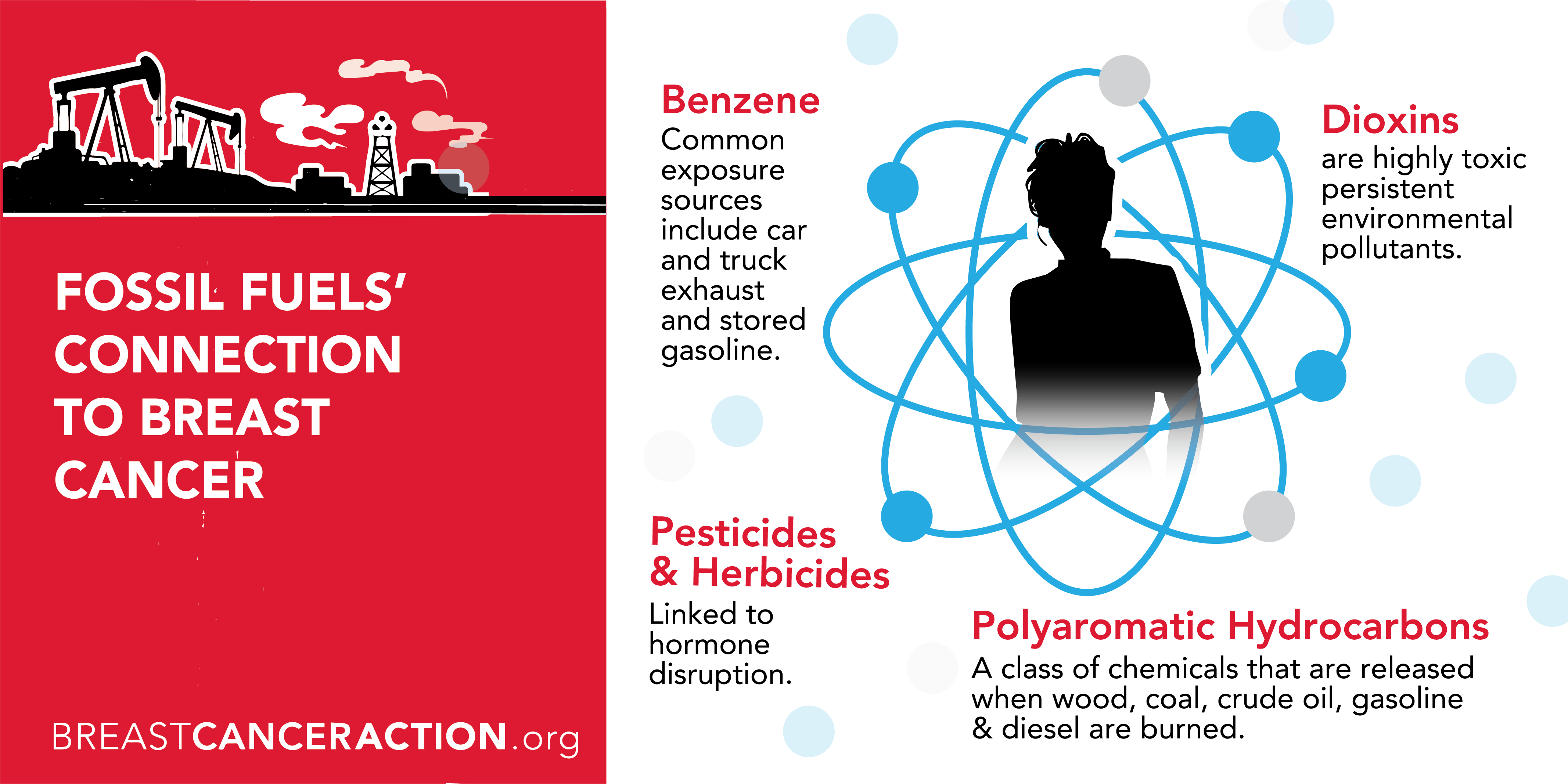
BCAction works to address and end breast cancer in ways far beyond the simple quick fix approach of increased screening and expanding access to healthcare. Broader solutions to eliminating inequities require policies that improve resources for schools in economically depressed neighborhoods; foster economic revitalization in low-income communities of color; and strengthen environmental protections and enforcement — these are some of the ways to directly impact the root causes of breast cancer inequities. At BCAction, we demand change such as strong regulatory reform to reduce exposures to harmful environmental toxins in all communities and we will always advocate for the necessary systemic changes that will end health inequities.
Breast Cancer Action recognizes that the breast cancer epidemic is a social justice issue. Breast cancer is a widespread health crisis that predominantly effects women in a male-dominated and profit-driven society, and addressing and ending the breast cancer epidemic requires profound changes at every level of our society.
In mainstream U.S. culture, breasts are linked to femininity, sexuality, and attractiveness. As a result, breast cancer is a highly sexualized and gendered disease. As a health justice organization with roots in the women’s health movement, we challenge the narrow definitions of femininity, womanhood, and sexuality that mainstream narratives about breast cancer impose on people at risk of and living with the disease. We recognize and honor the many ways people express their gender identity, including outside of the either/or of man/woman. We work to challenge mainstream assumptions about gender and sexuality as it relates to breast cancer risk, diagnosis, and treatment in order to make room for people of all gender identities in the breast cancer movement.
In our work for health justice, we strive to practice principled allyship by using the power and privilege we hold as an organization to build solidarity with communities who currently and/or traditionally have had less access to power, information, and resources.
The current breast cancer epidemic impacts communities unequally and leads to unacceptable differences in who develops breast cancer and when it develops, who gets high quality and timely treatment, and who dies from breast cancer. In order to address and end the breast cancer epidemic, we must tackle the root causes of these health inequalities, which are the result of a complex interplay of culture, power, economics, racism, and sexism.
Achieving health justice requires that each of us be free from oppressions that prevent all of us from living healthy lives in healthy communities. We believe that no single injustice can be effectively addressed in isolation, and we recognize that injustices in our society reinforce each other in many ways and at many levels.